 |
|
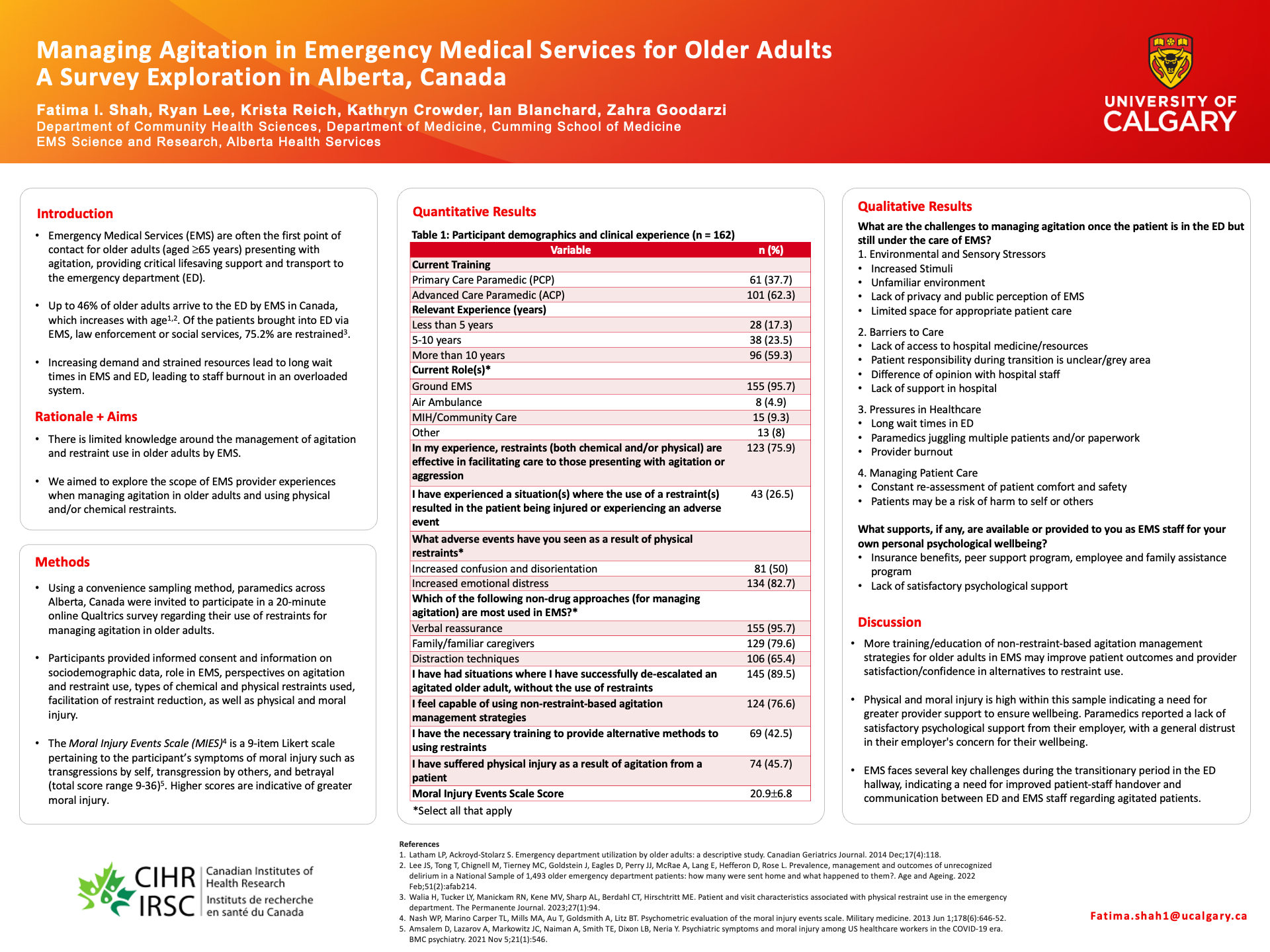
Title Managing Agitation in Emergency Medical Services for Older Adults: A Survey Exploration in Alberta, Canada Authors Fatima Shah, Ryan Lee, Krista Reich, Kathryn Crowder, Ian Blanchard, Zahra Goodarzi Introduction Emergency medical services (EMS) are often the first point of contact for agitated older adults, providing critical lifesaving support and transport to the emergency department (ED). However, there is limited knowledge available about the management of agitation and restraint use in older adults by EMS. Objective We aimed to explore the scope of paramedic experiences when managing agitated older adults and using physical and/or chemical restraints. Methods Paramedics (n=162) employed in Alberta, completed a mixed methods online survey, which queried socio-demographics, role(s) in EMS, agitation and restraint use in older adults, as well as physical and moral injury. Results The majority of our sample consisted of advanced care paramedics (62.3%), had more than 10 years of relevant EMS experience (59.3%), and worked in ground EMS (95.7%). Paramedics reported that older adults are restrained (both chemical and/or physical) due to risk of harm to self (81.5%) or others (76.5%), combative (73.5%), or the care team is unable to provide medical assistance due to resistance (58%). Most have not experienced a situation where restraint use resulted in patient injury or adverse event (71%), and 75.9% agreed that restraints are effective in facilitating care to those presenting with agitation or aggression. Verbal reassurance (95.7%), family/familiar caregivers (79.6%), and distraction techniques such as music and redirection (65.4%) were common non-drug approaches (for managing agitation) most used by EMS. Nearly half agreed that they had the necessary training to provide alternative methods to using restraints (45.2%), 89.5% agreed that they have successfully de-escalated an agitated older adult without using restraints, and 76.6% felt capable of using non-restraint-based agitation management strategies. Nearly half of all paramedics agreed that they have suffered physical injury as a result of patient agitation (45.7%). The mean total moral injury score was 20.9 ± 6.8 (range 9-35), and a lack of satisfactory psychological wellbeing support from the employer was reported. Conclusions A lack of older adult specific agitation management education calls for more training within EMS to improve patient outcomes and paramedic satisfaction. |
Fatima recently graduated with a Master of Science specializing in health services research from the University of Calgary. Her thesis focused on exploring the management of agitation in older adults in emergency medical services, drawing on a