|
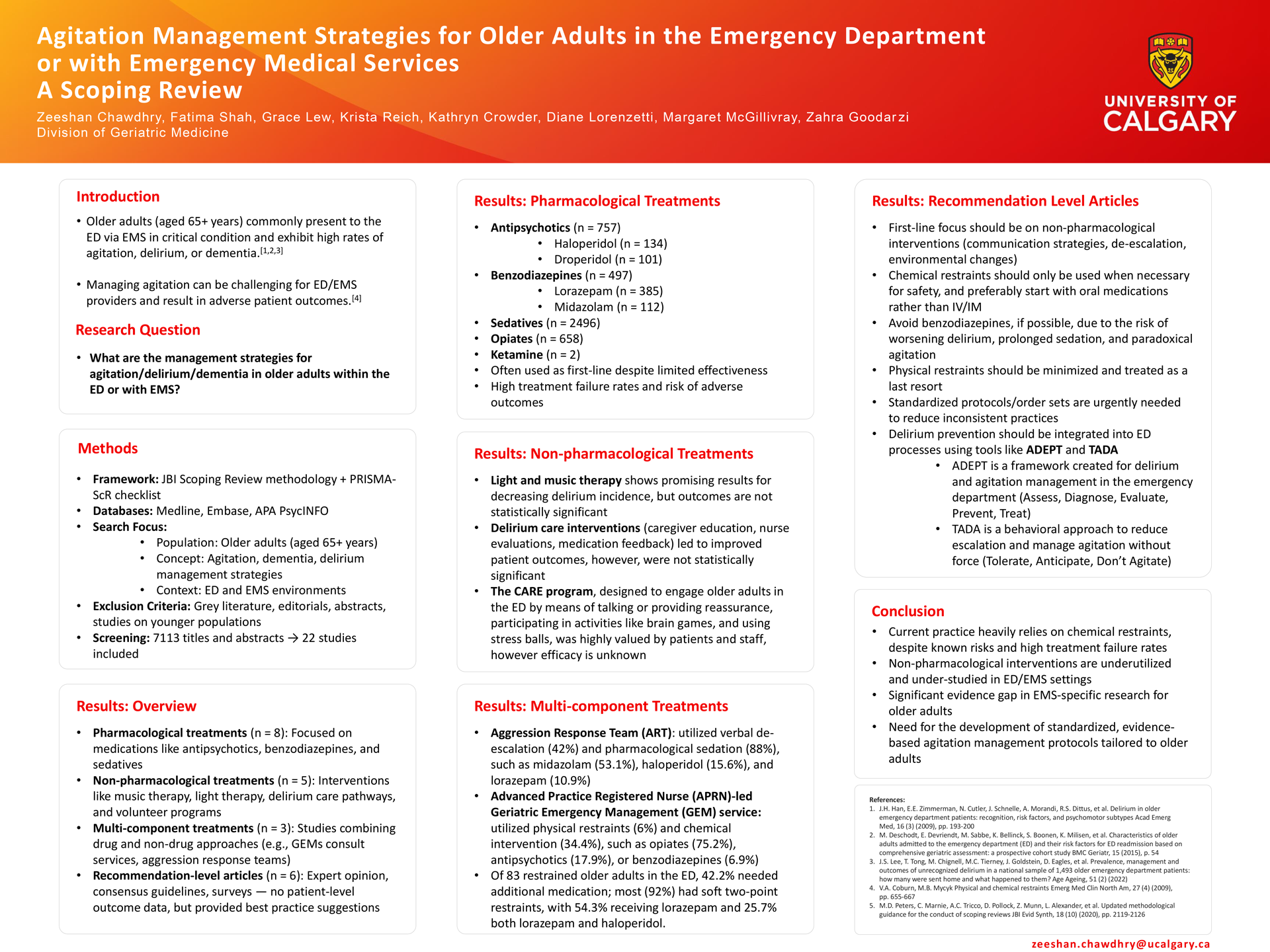
Introduction: Agitation is commonly encountered in emergency care environments, such as the Emergency Department (ED) and with Emergency Medical Services (EMS). Agitation poses significant challenges to patient care and safety for all involved. Older adults (aged 65+ years) commonly present to ED and EMS with agitation, delirium, or dementia, for which managing agitation can be challenging for ED/EMS providers and result in adverse patient outcomes. A scoping review of literature for approaches to the management of agitation in older adults in ED and EMS environments was completed.
Methods: We searched Medline, Embase, and APA PsycINFO, combining key words and subject headings for 3 concepts: “older adults, aged 65 and older,” “agitation/dementia/delirium,” and “ED/ EMS.” Studies which explored management strategies for agitation/dementia/delirium in older adults within the ED or EMS settings were included. Studies with younger populations (<65 years old) and/ or lacking patient data specifically from the ED or EMS environments were excluded.
Results: A total of 7113 studies were screened, of which 22 were included in this review: pharmacological (n=8), non-pharmacological (n=5), multi-component (n=3) treatments, and recommendations (n=6). Most were in the ED, and 5038 older adults were included across all studies. Antipsychotics and benzodiazepines to manage agitation were common. Non- pharmacological and multi-component interventions were less commonly evaluated and lacked exploration of patient outcomes. Recommendations stressed caution with pharmacological medications rather than prioritizing non-restraint strategies.
Conclusions: Most studies identified use of pharmacological treatment for agitation among older adults in ED/EMS settings, however, are not found to be overly effective and are associated with patient harm. There is a significant gap in evidence specific to EMS settings and evaluation of effectiveness of non-pharmacological interventions, highlighting the need for further research.
|