 |
|
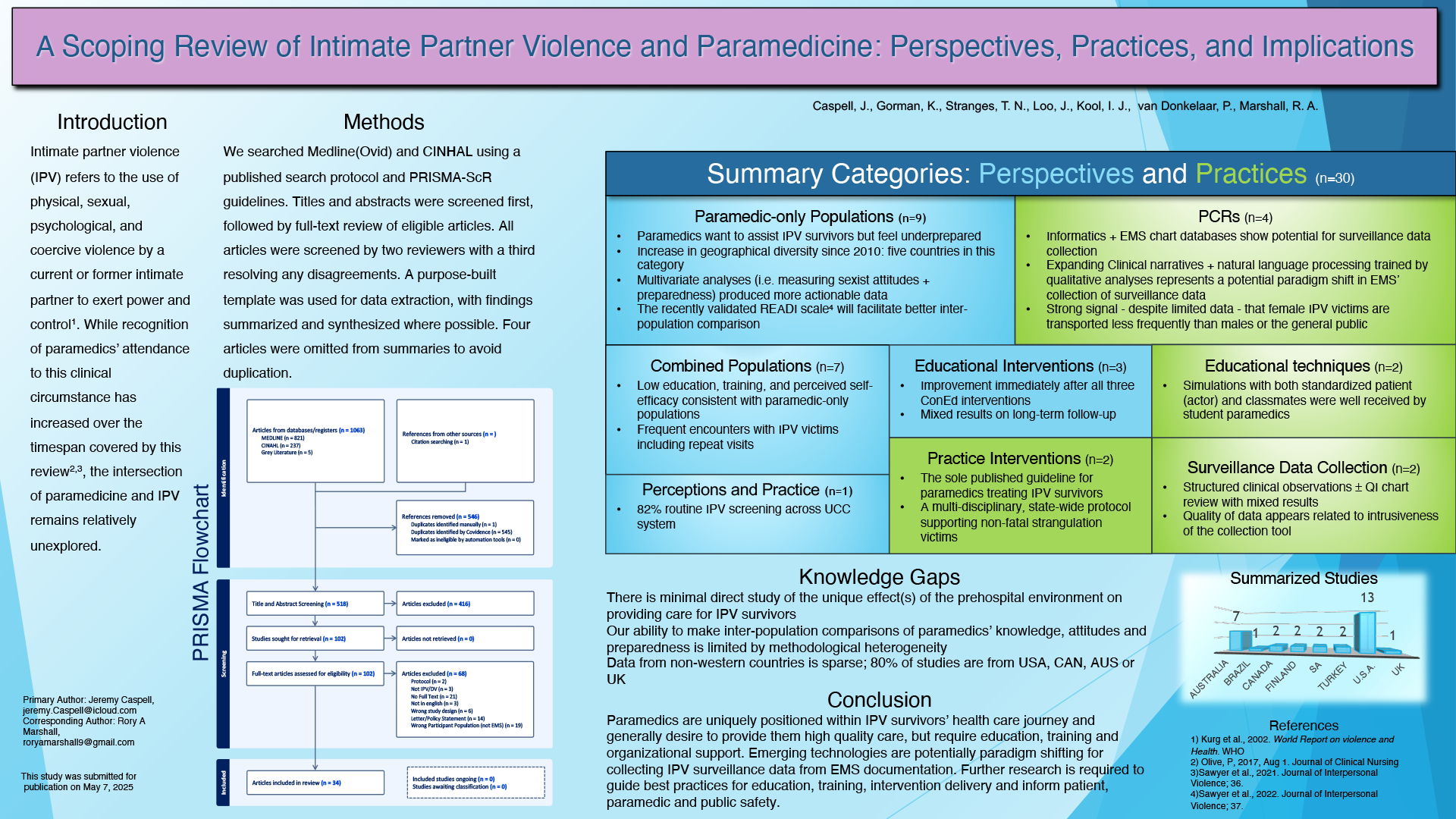
Title A Scoping Review of Intimate Partner Violence and Paramedicine: Perspectives, Practices, and Implications Authors Caspell, J.R.,1,2 Gorman, K.,3,4 Stranges, T. N.,4 Loo, J.,5 Kool, I. J.,5 van Donkelaar, P.,4 Marshall, R. A.4,6
Introduction Intimate partner violence (IPV) is increasingly being recognized as a clinical circumstance to which paramedics attend. IPV refers to the use of physical, sexual, psychological, and coercive violence by a current or former intimate partner to exert power and control. The intersection of paramedicine and IPV remains largely unclear. Objective To provide a comprehensive synthesis of the available evidence at the intersection of paramedicine and IPV. Methods This review followed a published protocol (Open Science Framework), and PRISMA-ScR guidelines. Co-developed with two trained librarians, a search strategy was used to locate potential articles in MEDLINE, CINAHL, and gray literature. Included articles examined perceptions and/or practice of paramedics and students in the context of IPV. Titles and abstracts were screened by two reviewers, followed by full text reviews when eligible; a third reviewer resolved any disagreement. Data were extracted using a purpose-built template. Findings were summarized and synthesized. Results Of the 517 articles, 34 were included. The literature was varied and heterogenous, preventing mass, detailed synthesis. Generally, paramedics were motivated to assist IPV survivors but perceived their education as insufficient to provide high-quality care, reporting low rates of training/education with corresponding low self-efficacy. Considerations for the specific and unique environment of paramedicine were lacking. Standardized patients and/or simulations were beneficial for student paramedics acquiring history gathering and interview skills. Jurisdictional variations in legislation, policy, and standards, as well as overlapping agency/department regulations introduced practice variance. The validity and utility of paramedic surveillance data collection were unclear. However, it appears female IPV survivors were less likely to be transported to hospital versus male IPV survivors or non-IPV population averages. Conclusions Paramedics were recognized as a poorly understood, under-utilized, and under-equipped resource for IPV survivors. Despite this recognition, current literature is insufficient to comprehensively guide practice. Limited quantity, utility, and heterogeneity contribute to this challenge. Future research should leverage newly developed and validated measures to identify gaps responsive to educational and/or policy interventions and explore novel technologies to improve the quality of paramedic-collected IPV data. Equipping paramedics with the tools to provide high-quality IPV care will benefit IPV survivors, paramedics, and society. |
Jeremy Caspell is an Advanced Care Paramedic with Alberta Health Services EMS and currently completing a Bachelor of Health Sciences at Thompson Rivers University.