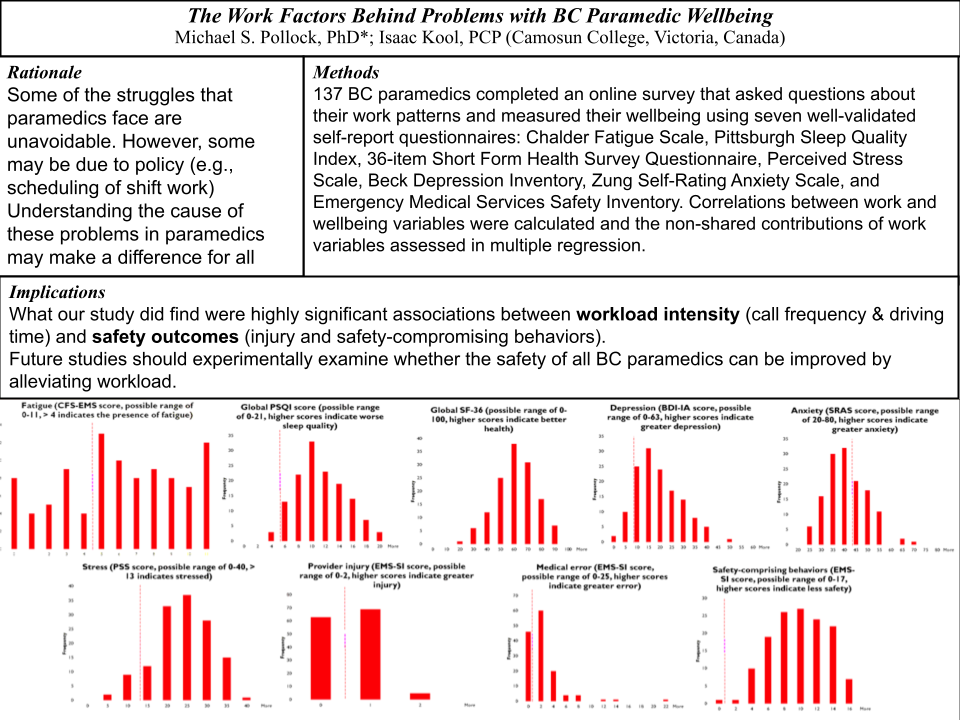
The Work Factors Behind Problems with BC Paramedic Wellbeing
Objectives: Paramedics around the world commonly suffer issues with their wellbeing - such as increased fatigue and poorer sleep quality, mental health, and safety outcomes – and these problems have been linked to the timing and duration of shift work. The purpose of this study was to assess the wellbeing of BC paramedics and to examine their associations with work factors.
Methods: 137 BC paramedics completed an online survey that asked questions about their work patterns and measured their wellbeing using seven well-validated self-report questionnaires: Chalder Fatigue Scale, Pittsburgh Sleep Quality Index, 36-item Short Form Health Survey Questionnaire, Perceived Stress Scale, Beck Depression Inventory, Zung Self-Rating Anxiety Scale, and Emergency Medical Services Safety Inventory. Correlations between work and wellbeing variables were calculated and the non-shared contributions of work variables assessed in multiple regression.
Results: On average, BC paramedics show worse levels of wellbeing (for fatigue, sleep quality, health, depression, and safety outcomes) than previously reported for paramedics elsewhere. While these problems could not be accounted for by shift work patterns (shift frequency, shift duration, total shift time, rotational shifts, night shifts, number of days on to days off), safety outcomes (provider injury and safety-compromising behavior) were associated with indicators of increased workload intensity, such as increased on-job driving time and calls per shift. In contrast to the worse safety outcomes with increased workload, choosing to work greater numbers of days consecutively showed better wellbeing outcomes (less fatigue, better sleep quality, and better overall health) in some full-time paramedics (termed “super full-timers”).
Conclusions: Future studies should experimentally examine whether the safety of all BC paramedics can be improved by alleviating workload and further investigate the characteristics of these super full-timers that allow them to work longer and yet live healthier.
 |
About the author:
 |
| Isaac Kool is a Primary Care Paramedic with BC Emergency Health Services who is currently working on a BSc in Biopsychology at Camosun College/University of Victoria. Isaac Kool has been involved with the Critical Incident Stress (CIS) team for almost three years. Over Isaac's time with the CIS team, he gained interest in the wellness of BC paramedics with the hope of possibly finding solutions in the future. |



Commentary