The Use of Sedation in the Management of Non-invasively Ventilated Pediatric Patients During Out-of-hospital Transport by BCEHS Infant Transport Team Paramedics
|
Principle Investigator: Brian Thornburn CCP-ITT, BSc, RRT
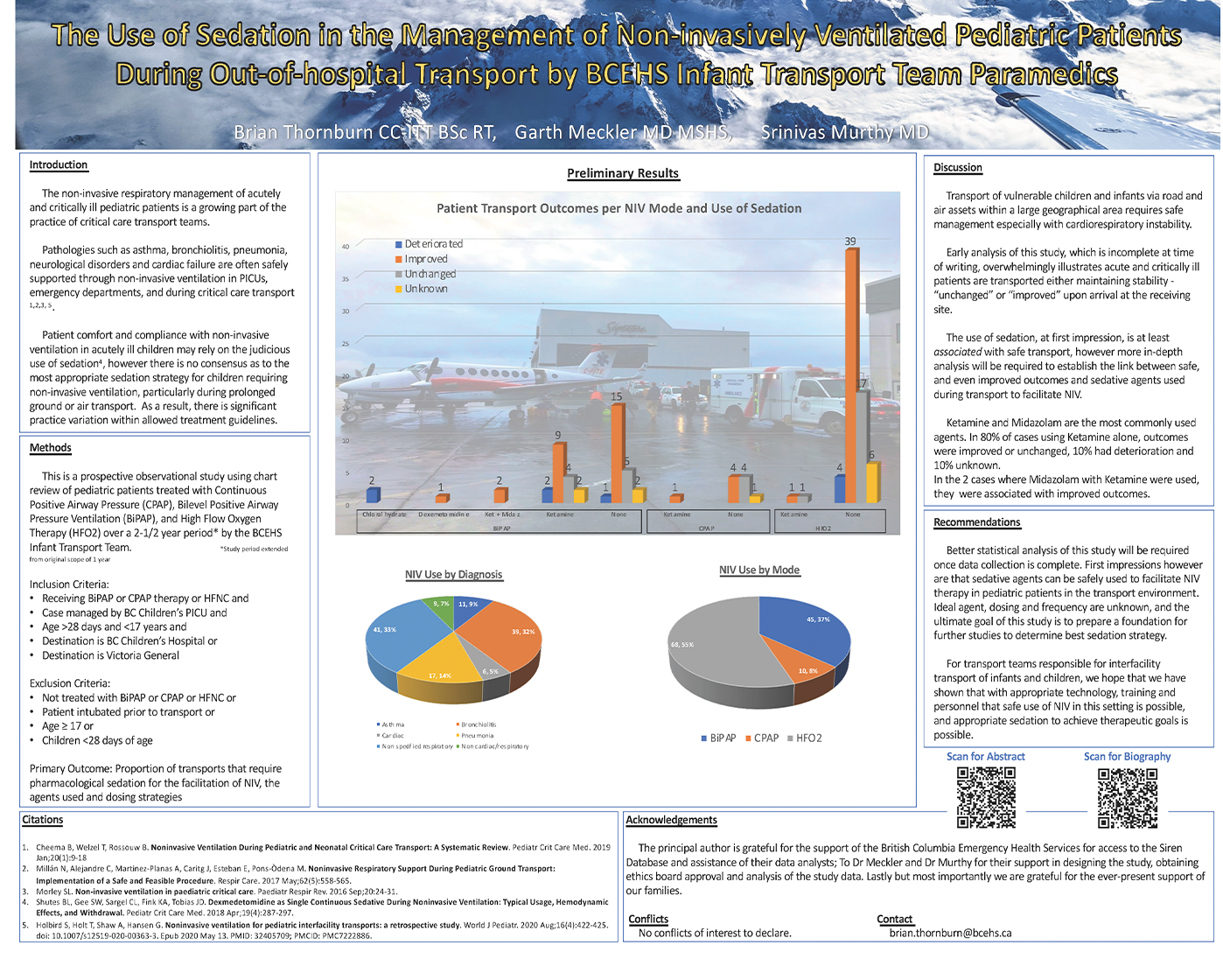
Background The non-invasive respiratory management of acutely and critically ill pediatric patients is a growing part of the practice of Critical Care Transport Teams. Pathologies such as asthma, bronchiolitis, pneumonia, neurological disorders and cardiac failure are often supported through non-invasive ventilation in PICUs, emergency departments, and during critical care transport1,2,3. Patient comfort and compliance with non-invasive ventilation in acutely ill children may rely on the judicious use of sedation4, however there is no consensus as to the most appropriate sedation strategy for children requiring non-invasive ventilation, particularly during prolonged ground or air transport. As a result, there is significant practice variation within allowed treatment guidelines. The BCEHS Infant Transport Team (ITT) is a paired paramedic model with specialized neonatal, pediatric and maternal critical care training. The team operates under the direction of physician advisers specialized in NICU, PICU, maternofetal and pediatric emergency medicine. This team operates via land or air, 24 hours a day, covering a large land-mass with significant geographic and weather related challenges. There are several manuscripts describing pediatric non-invasive ventilation in the acute, critical care and transport setting1,2,3. Also, there are several studies describing pharmacological management during pediatric non-invasive ventilation4. There is however a paucity of literature describing the optimal agents and dosing of pharmacological sedation for non-invasively ventilated pediatric patients in the transport setting4. The BC Infant Transport Team is a unique service that manages critically ill infants and children in austere environments and long air and ground transports, and objective information on the safety and efficacy of pharmacologic sedation for non-invasive ventilation in this population is needed in order to provide optimal care. Objectives:
We aim to gather data for a period of one year, through access to the Paracare Siren database. Data collection will start at time of appropriate approvals and continue for one year. [Due to the Covid-19 pandemic, case numbers decreased significantly. Approvals were granted twice to extend the study to 2 –½ years.] Inclusion criteria is to include all patient > 28 days age transported via ITT who have non-invasive ventilation (NIV) provided during transport. NIV is defined as BiPAP, CPAP, or high-flow oxygen therapy. Exclusion criteria include children with endotracheal intubation and mechanical ventilation prior to arrival of ITT for transport, as well as neonates (<28 days age) or older adolescents (≥17 years). Data will be prospectively collected by the transporting team. Data elements to be extracted include baseline demographics (age, gender, weight), co-morbidities, , mode of non-invasive ventilation (CPAP, BiPAP, hi-flow NC), pharmacologic agent(s) and dose(s) used or sedation, as well as any during transport. Sedation will be titrated according to ITT protocol, using a RASS score for standardized assessments of agitation, as per current standard of care. All data are routinely recorded in the ePCR as per standard BCEHS documentation practice. This will be a descriptive evaluation of current practice, and formal comparative statistics will not be performed. This will provide a baseline for future studies. Methods Hypothesis: The use of sedative agents to ensure effective non-invasive ventilation for select pediatric patients can be provided safely in the transport environment by ITT trained paramedics. Study Design: prospective observational study using chart review of pediatric patients treated with Continuous Positive Airway Pressure Bilevel Positive Airway Pressure Ventilation, and High Flow Nasal Cannulae over a 12-month period* by the BCEHS Infant Transport Team. *exended as previosuly explained Study Subjects: All children >28 days and <17 years of age transported by the BCEHS ITT from January 1 2020 - June 31 2022 will be screened for inclusion / exclusion criteria. Inclusion Criteria:
Exclusion Criteria:
Primary Outcome: Proportion of transports that require pharmacological sedation for the facilitation of NIV, the agents used and dosing strategies Secondary Outcomes:
3) Data Collection: All transport data will be generated from the Medusa Siren database maintained by the BC Emergency Health Services. Follow up outcome data will be from charts identified as following the identified transports to BC Children’s Hospital Patient Care Reports during the study period with BiPAP or CPAP therapy indicated will be screened for inclusion and exclusion criteria as above. Data will be collected using an automated report generating mechanism and will include the following variables:
Results Data collection is still ongoing. Will present preliminary results if selected for presentation. References:
|
About the author:
 |
|
Brian Thornburn, a paramedic currently specializing in the Critical Care Transport of neonatal, pediatric, and maternal patients has worked with British Columbia Ambulance Service, in a variety of roles for over 25 years. The Infant Transport Team is a specialized Critical Care division of Clinical Services and Air Operations and functions in partnership with BC Children’s Hospital and BC Women’s Hospital. As a member of ITT, Brian responds to requests for interfacility transport of neonatal, acute, and critically ill pediatric and high- risk maternal patients. The team responds throughout British Columbia, a land area of over 990,000 square kilometers on the West Coast of Canada. Working as a team composed of two ITT licensed Paramedics, paramedics provide critical interventions and intensive care for patients. On occasion ITT will also utilize physicians as part of their fellowship training with BC Children’s Hospital PICU or BC Women’s Hospital NICU. Brian’s extensive training and career have included work as an instructor, preceptor and mentor of ITT students, physicians, nurses, and respiratory therapists, produced in-services, planned, and implemented projects, evaluated, implemented, and trained staff in new technology, conducted research, and acted as station Unit Chief. Brian’s ongoing continuing medical education has been complemented by a Bachelor of Science in General Science with a Biology Minor from the University of Waterloo (1997), a Diploma in Respiratory Therapy from Thompson River’s University (2002) and Infant Transport Team Program completion from BCEHS (2013).
Brian deeply values being in service to the community. His career has focused on mandates of health, well-being, and service to community. Brian is an avid volunteer in sporting events, charitable organizations, and public relations. Brian strives for excellence and works to enable others to meet their personal and professional goals. Brian also loves to spend time being active in the outdoors as well as designing and creating indoor and outdoor home projects. |



Commentary