|
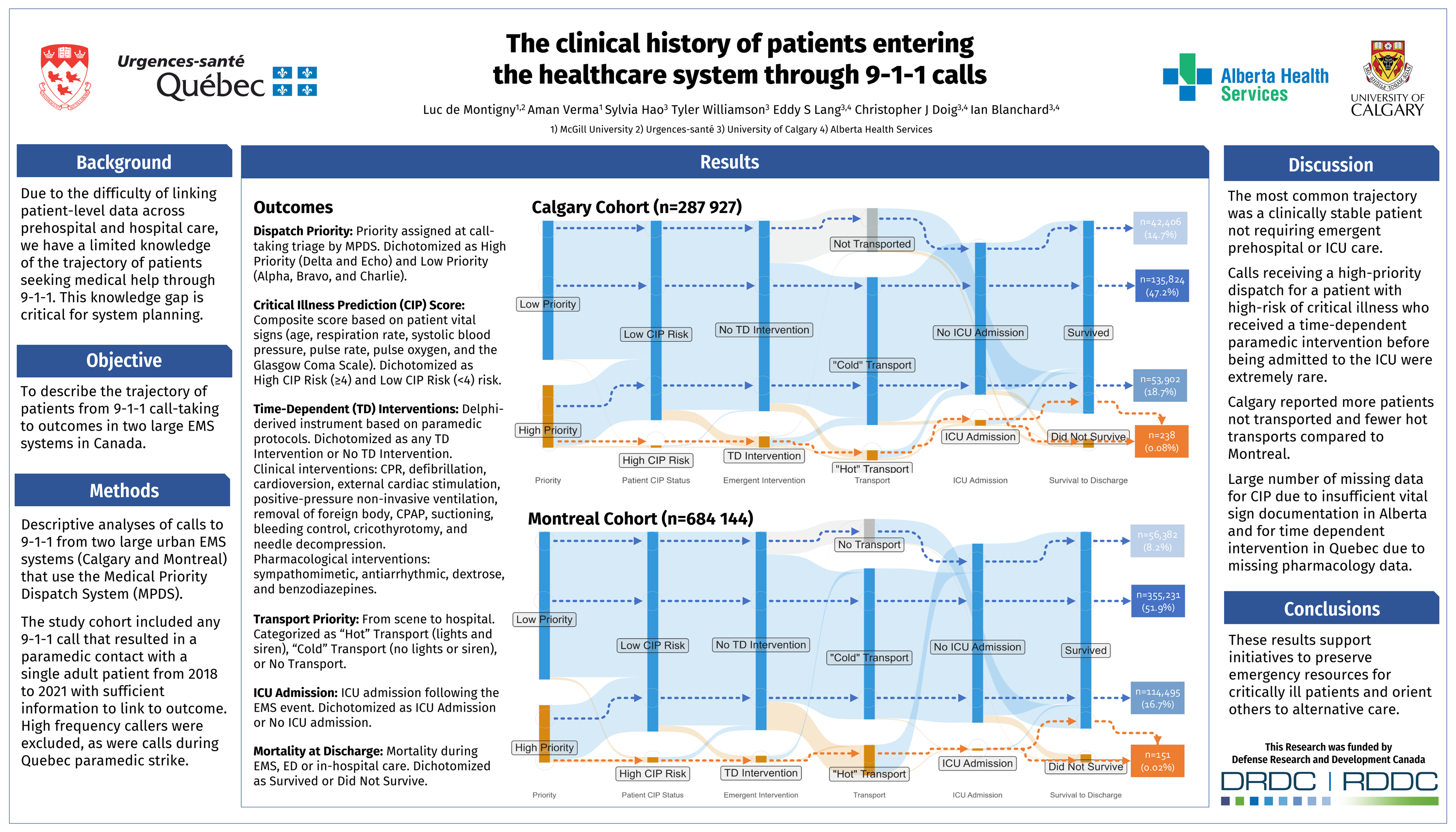
The Clinical History of Patients Entering the Healthcare System through Medical 9-1-1 Calls de Montigny, L; Verma, A; Hao, S; Williamson, T; Lang, ES; Doig, CJ; Blanchard, IE Introduction: Due to the difficulty of linking patient-level data across prehospital and hospital care, we have a limited knowledge of the trajectory of patients seeking care through 9-1-1. This knowledge gap inhibits an understanding of the relationship between call-taking, paramedic interventions, and post-transport outcomes, which is critical for system planning. Objective: To describe the trajectory of patients from 9-1-1 call-taking to outcomes. Methods: Descriptive analyses of calls to 9-1-1 from two large urban EMS systems (Quebec [QC] and Alberta [AB]) that use the Medical Priority Dispatch System (MPDS) for call-taking triage. The study cohort included all 9-1-1 calls for adult patients from 2018 to 2021 with sufficient information to link to outcome. The dataset included patient acuity on scene (Critical Illness Prediction score [CIP]; time-dependent paramedic intervention), and post-transport outcomes (ICU admission; all-cause mortality at discharge). Results: A total of 611 125 calls were included (QC=323 198; AB=287 927). QC reported 28.7% as high priority (Delta/Echo) and 71.2% as low priority (Alpha/Bravo/Charlie); AB reported 31.0% and 69.0% respectively. High risk of critical illness (CIP=4–8) was 2.0% (QC) and 1.0% (AB), 1.4% (QC) and 5.6% (AB) received at least one time-dependent paramedic intervention, ICU admission was 1.2% (QC) and 2.9% (AB), and all-cause mortality was 3.8% (QC) and 4.4% (AB). The most common patient trajectory was the low-priority call for a patient with low-risk of critical illness who received no time-dependent paramedic interventions, was not admitted to the hospital, and did not die (QC=48.3% and AB=30.0%). High-priority calls for a patient with high-risk of critical illness who received a time-dependent paramedic intervention and was admitted to the ICU were rare (high priority: QC=0.03% and AB=0.06%). Conclusion: The most common trajectory was a clinically stable patient not requiring emergent prehospital or ICU care. These results support initiatives to preserve emergency resources for critically ill patients and orient others to alternative care. |
Dr. Luc de Montigny is a research advisor at Urgences-santé, one of Canada's largest emergency medical systems, where he coleads the research program, manages collaborative studies, and develops internal capacity and projects
Ian Blanchard has worked in Emergency Medical Services (EMS) systems in Canada and the United Kingdom for the last twenty five years in various capacities, including as an Advanced Care Paramedic, quality assurance strategist, and researcher.
Aman Verma is a Research Associate at the Surveillance Lab, where he is actively involved in several research projects involving large healthcare databases. Aman is currently involved in research applying machine learning to emergency medical service