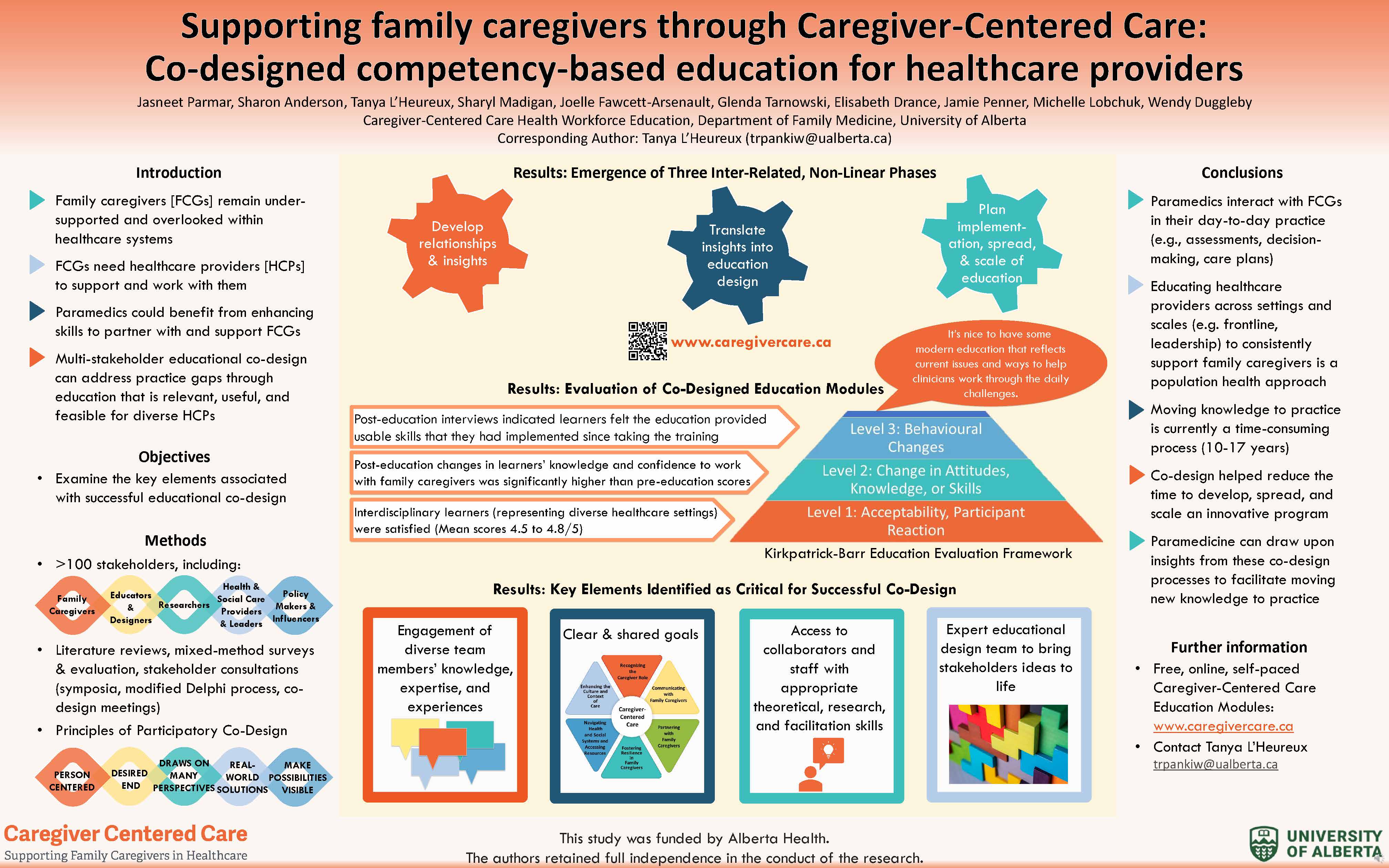
Supporting family caregivers through Caregiver-Centered Care: Co-designed competency-based education for healthcare providers
|
Authors: Jasneet Parmar, Sharon Anderson, Tanya L’Heureux, Sharyl Madigan, Joelle Fawcett-Arsenault, Glenda Tarnowski, Elisabeth Drance, Jamie Penner, Michelle Lobchuk, Wendy Duggleby Introduction: Moving integrated care closer to home for people living with complex conditions is highly dependent on healthcare providers supporting and working with family caregivers. While family caregivers provide 70-90% of the care for people living in the community, they are under-supported and overlooked within healthcare systems. Educating interdisciplinary healthcare providers to support diverse family caregivers throughout their care trajectories is a necessary step towards addressing an inconsistent system of supports. Involving multi-level stakeholders in the educational co-design process can help move knowledge into practice and ensure education is relevant, useful, and feasible for diverse healthcare providers. Objective: This research examines the key elements and research tools associated with successful educational co-design. Methods: Over 100 stakeholders including family caregivers, educators, researchers, health and social care providers and leaders, educational designers, and policymakers were involved in the three co-design phases to develop health workforce education to support family caregivers. The phases were: 1) Developing relationships and insights; 2) Translating insights into the design of the education; and 3) planning the implementation, spread, and scale-up of education. Each phase used research tools, including literature reviews, qualitative and quantitative survey research on specific topics, stakeholder consultations (symposia, modified Delphi process, co-design meetings), and mixed methods evaluation. Results: Modules have been highly accessed by healthcare providers and trainees. Interdisciplinary learners reporting very high satisfaction, relevance, and usefulness as well as significant knowledge and confidence gains upon completion. Four key elements were critical to successful co-design include: 1) engagement of diverse team members’ knowledge, expertise, and experiences; 2) clear and shared goals (e.g. competency framework); 3) co-design team access to collaborators and staff with appropriate theoretical, research, and facilitation skills; and 4) an expert educational design team to bring stakeholders’ ideas to life. Conclusion: Paramedicine can draw upon insights from co-design processes to facilitate moving new knowledge to practice, which is currently a time-consuming process (10 to 17 years). We leveraged stakeholders’ knowledge, experiences, and insights to reduce the time to develop, spread, and scale an innovative population health approach in which interdisciplinary healthcare providers with diverse experiences are educated to support all family caregivers throughout diverse care trajectories. |
About the lead author:
 |
| Dr. Jasneet Parmar, Professor, Department of Family Medicine, Faculty of Medicine and Dentistry, University of Alberta is a Care of the Elderly Physician. She is the Program Lead for Caregiver-Centered Care Health Workforce Education, a Program of Applied Research &Innovation in Health Services Delivery in Family Caregiving, Department of Family Medicine, University of Alberta. Email: Jasneet.parmar@albertahealthservices.ca |



Commentary