|
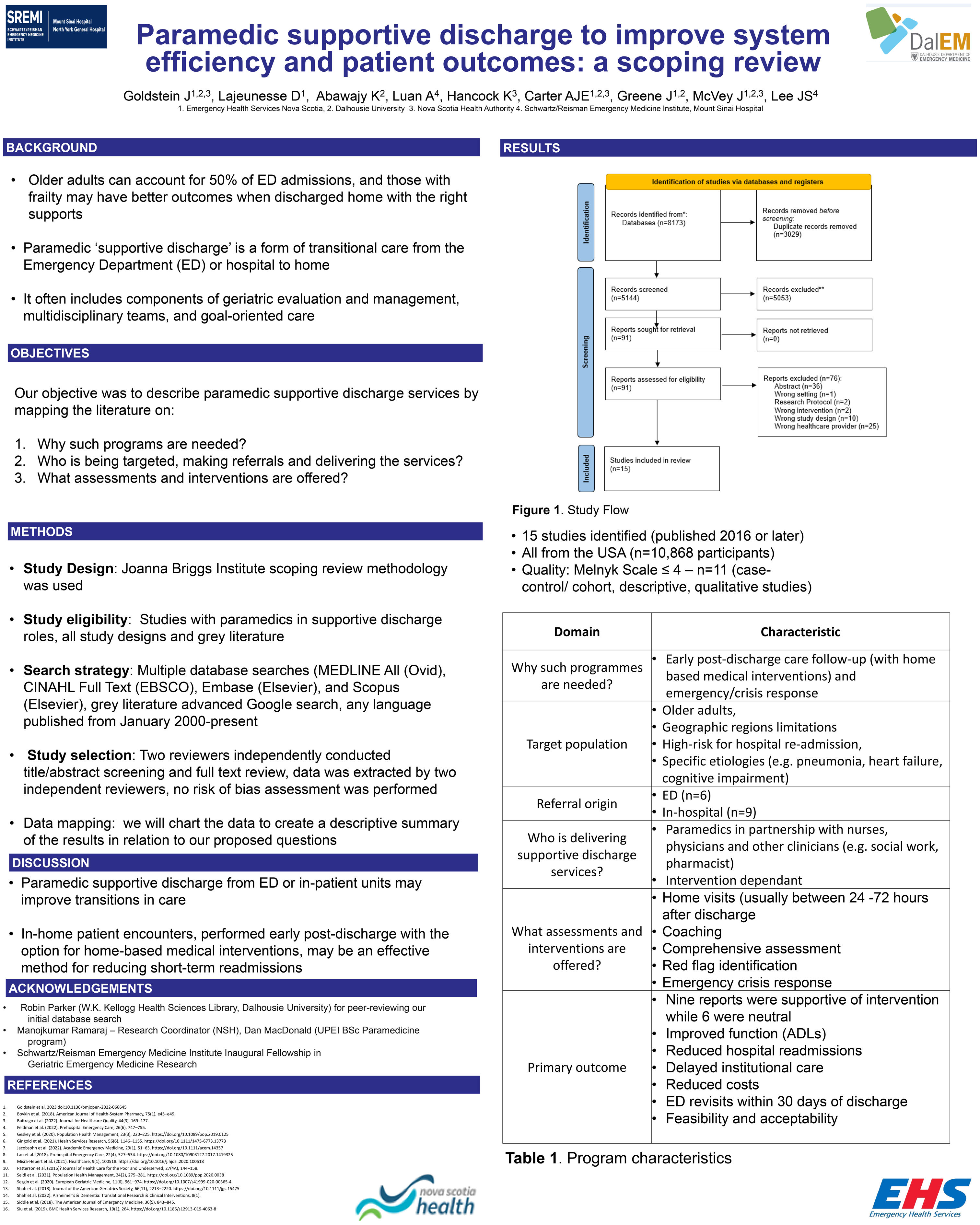
Paramedic supportive discharge to improve system efficiency and patient outcomes: a scoping review Author List: Judah P Goldstein PhD1 Dominic Lajeunesse 2 Khadija Abawajy BSc1 Angela Luan BSc3 Kristy Hancock4, Alix Carter MD MPH2, Jennifer Greene BSc2 Jennifer McVey MD MSc2 Jacques Lee MD MSc3 Keywords: community paramedic, geriatrics, frailty, supportive discharge, transitions in care Author Affiliations: 4. Maritime SPOR SUPPORT Unit Abstract: Introduction: Complex discharges of older people are problematic. Paramedics could help by adding an option for in-home assessment/ intervention post discharge. Our objectives were to identify paramedic supportive discharge programs from the ED/ hospital to reduce avoidable hospital admissions. Methods: We included studies on expanded paramedic scope and roles post discharge from the ED/ hospital. There was no language exclusion. We used the Joanna Briggs Institute methodology and reported using PRISMA-ScR criteria. We used a search strategy designed by a health science librarian for eligible studies from 2000 to present. Studies were included if they incorporated a paramedic during the transition from ED or hospital to home. Two independent reviewers conducted screening and full text review. One reviewer extracted data and another verified. Findings are reported descriptively. Results: We identified 5144 records and included 15 reports: 3 randomized controlled trials (from a single study), 4 program descriptions, 6 observational reports, 1 scoping review, and 1 qualitative study. All studies were published in 2016 or later and were from the United States and included patients (n=10,868) who were referred from either the ED (n=6) or in-hospital unit (n=9). Seven unique programs were identified and included variations of a modified Care Transition Intervention (CTI), Hospital at Home (HaH) service, transitional care strategy, or disease specific transitional care program (e.g. heart failure). Most services targeted older adults, living in specific geographic locations, at high risk for hospital readmission or with specific etiologies (e.g. pneumonia, heart failure, cognitive impairment). Paramedics provided early post-discharge care follow-up (with home based medical interventions) and emergency/crisis response in partnership with nurses, physicians and other clinicians (e.g. social work, pharmacist). Post-discharge care included home visits (n=15), coaching (n=7), comprehensive assessment (n=4), referral to other services (n=4), and red flag identification (n=5). Emergency/crisis response (n=3), functional and mobility assessment (n=3) were also described. Interventions were deemed effective in 9 reports while 6 were neutral. Conclusion: Paramedic supportive discharge services might be able to address gaps within the health care system. Further research is needed to understand who might benefit most from this type of care. |
Dr. Judah Goldstein is the Research Coordinator for Emergency Health Services, Nova Scotia. Dr. Goldstein is a Primary Care Paramedic and has worked in the EHS ground ambulance system since 2000.