 |
|
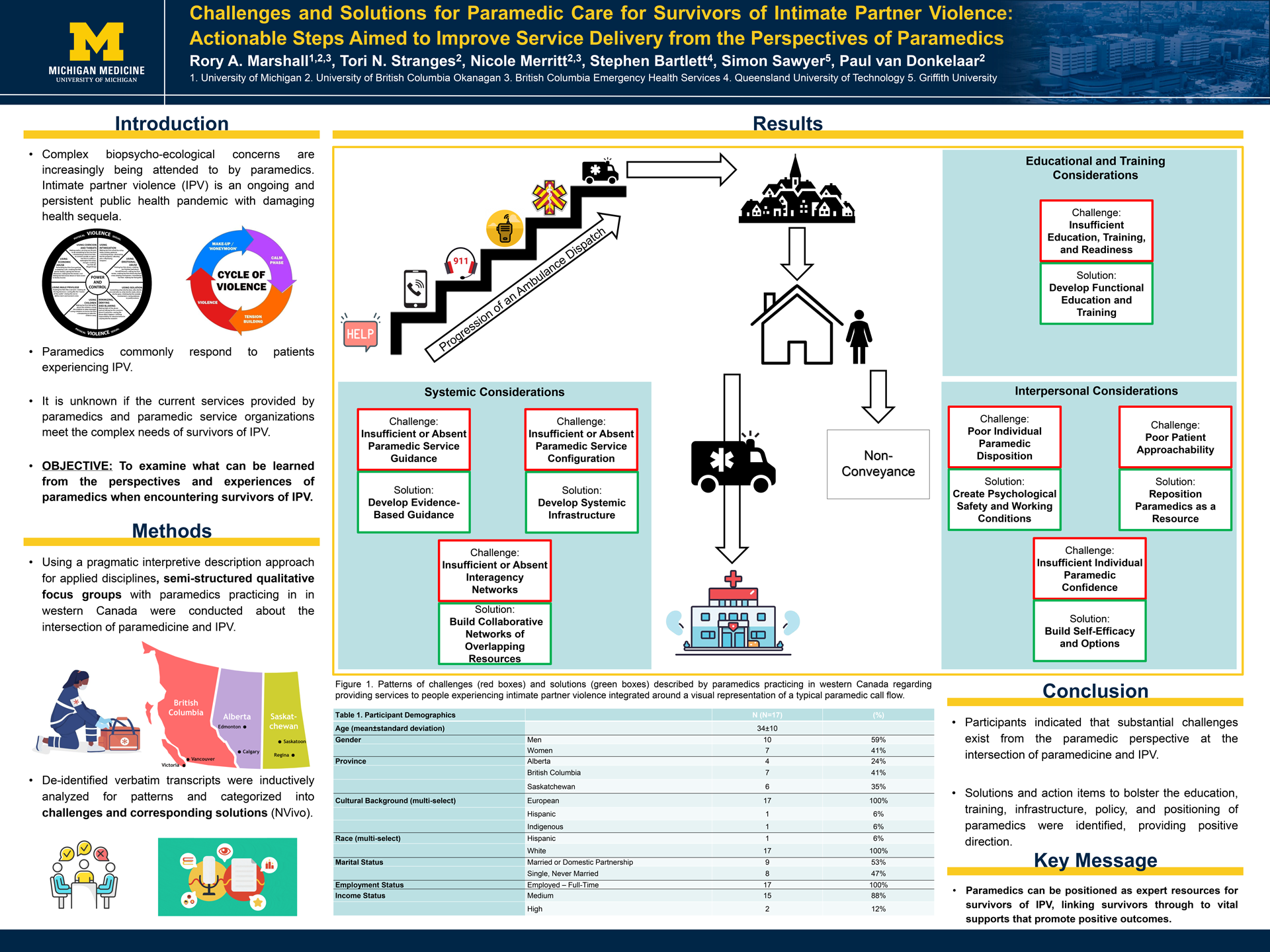
TITLE: Challenges and Solutions for Paramedic Care for Survivors of IPV: Actionable Steps Aimed to Improve Service Delivery from the Perspectives of Paramedics Rory A. Marshall1,2, Tori N. Stranges2, Nicole Merritt1,2, Stephen Bartlett3, Simon Sawyer4, Paul van Donkelaar2
INTRODUCTION: Complex biopsycho-ecological concerns are increasingly being attended to by paramedics. Intimate partner violence (IPV) is an ongoing and persistent public health pandemic with damaging health sequela. Paramedics commonly respond to patients experiencing IPV. It is unknown if the current services provided by paramedics and paramedic service organizations meet the complex needs of survivors of IPV. OBJECTIVE: To examine what can be learned from the perspectives and experiences of paramedics when encountering survivors of IPV. METHODS: Using a pragmatic interpretive description approach for applied disciplines, semi-structured qualitative focus groups with paramedics practicing in in western Canada were conducted about the intersection of paramedicine and IPV. De-identified verbatim transcripts were inductively analyzed for patterns and categorized into challenges and corresponding solutions (NVivo). RESULTS: N=17 paramedics (Women n=7 (41%), Men n=10 (59%); Mean Age 34±10 years) participated in four focus groups. Even without clinical practice guidance for IPV, participants felt the service they were providing did not meet the needs of survivors. Common challenges at the intersection of paramedicine and IPV were: 1) patient approachability, 2) individual paramedic disposition, 3) individual paramedic confidence, 4) paramedic service education, training, and readiness, 5) paramedic service guidance, 6) paramedic service configuration, and 7) interagency networks. Solutions and action items to address each challenge included updated functional education, training, infrastructure, and policy. CONCLUSIONS: Participants indicated that substantial challenges exist from the paramedic perspective at the intersection of paramedicine and IPV. Solutions and action items to bolster the education, training, infrastructure, policy, and positioning of paramedics were identified, providing positive direction. Meaningful, evidence-based implementation of these results should be pursued to advance the profession. Paramedics can be positioned as expert resources for survivors of IPV, linking survivors through to vital supports that promote positive outcomes. |
Rory A. Marshall is a PhD Candidate in the Faculty of Health and Social Development at the University of British Columbia Okanagan. He completed his MSc in Biomedical Sciences at the University of Saskatchewan and his BA in Kinesiology and Business